Is Ivermectin Beneficial for Ventilator-Induced Acute Respiratory Distress Syndrome (ARDS)?
Background: In March and April 2020, employees at Beth Israel Medical Center noticed a problem with blood clots among ventilated patients which they described as ARDS: Acute Respiratory Distress Syndrome. Their solution was to try an anti-coalgulent tPA: Tissue Plasminogen Activator. (1) (2) (3).
I do not have any information on if the tPA was a successful treament.
I have a question that I am soliciting medical opinions on. Would Ivermectin have been useful in treating the blood clots resulting from ventilator-induced ARDS? (I know some may wish to argue that “COVID” caused the ARDS, but ARDS has been a common result of using ventilators for any reason long prior to “COVID.”)
Ivermectin is comprised of synthetic excretions of Streptomyce avermectinius called “avermectins.” S. avermitilis was found in soil by Satosh Ōmura as part of a collaboration with Merck.
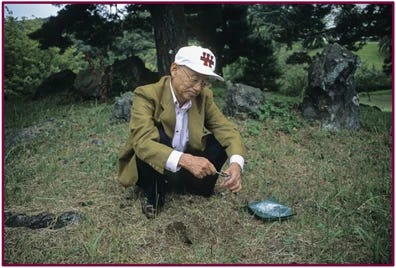
Pictured: Satoshi Ōmura collecting soil from the very site where the fateful sample containing Streptomyces avermectinius (S. avermitilis) was taken in 1973
Ivermectin is antibacterial (4), although there’s not much scientific literature on the antibacterial qualities.
Bacteria also plays a major role in the blood clots associated with ARDS. According to at least one paper, “Coagulation (blood clotting) becomes activated by circulating endotoxin or bacteria..” Here’s more text from the reference:
Coagulation and inflammation in acute lung injury, 2002
The acute respiratory distress syndrome (ARDS) is a severe lung injury in patients with sepsis and other acute inflammatory insults, which is characterized by fibrin deposition in the pulmonary parenchyma, vasculature, and airspaces. Recent evidence suggests that progressive ARDS is closely linked to activation of inflammation and coagulation. Coagulation becomes activated by circulating endotoxin or bacteria, and a procoagulant state develops in the vascular and the alveolar compartments of the lung. This state is Tissue Factor (TF)-dependent and associated with increased elaboration of inflammatory cytokines. A similar procoagulant state is found in bronchoalveolar lavage of patients with ARDS, suggesting that extravascular coagulation contributes to lung inflammation. TF and other coagulation proteins, including Factor Xa, thrombin, and fibrin, also contribute to the pathogenesis of acute lung injury through multi-level interactions with inflammatory effectors, in which these proteins coordinately act as regulators of tissue injury responses. Each coagulation protein has direct and independent effects on inflammatory events that influences lung injury through changes in cytokine elaboration, inflammatory cell migration and activation, surfactant function, and repair mechanisms. New interventional strategies directed at procoagulant activity highlight the importance of the coagulation system to acute lung injury and suggest that blockade of initiation of coagulation may have therapeutic benefit in patients with ARDS.
There are numerous other articles which reference the role of bacteria in blood clots and ARDS. My question once again is, is Ivermectin beneficial against these blood clots? If Ivermectin killed the circulating bacteria, would the bacteria have been unable to “activate” the blood clots? Would it at have cut down on the high mortality rated of the ventilated “COVID” patients?
Dr. Mary Bowden wrote Ivermectin prescriptions for hospitalized COVID patients which others tried to force hospitals to administer under court order. Dr. Bowden made a statement on Twitter about this effort to save lives:
The Statement of Dr. Mary Bowden on the Mortality Rates of Hospitalized COVID Patients who were and were not Administered Ivermectin under Court Order
From Twitter, February 27, 2023. I reconnected w/ (Beth Parlato) over the weekend…hero lawyer who represented Jason Jones and his wife. She and co-counsel Ralph Lorigo filed 189 cases for hospitalized patients trying to get ivermectin. 80 cases went to hearings/trial. They won about 40 and lost about 40.
Over 90% of the patients who were administered Ivermectin under court order lived. The ones that did not receive the Ivermectin all died.
I do not have the data on how many of these patients were ventilated or had ARDS blood clotting issues. In any case it is noteworthy that the Ivermectin worked somehow.
So with that I’ll conclude and hopefully start a productive discussion about Ivermectin and ARDS.
Charles Wright
REFERENCES:
(1). March 26, 2020. New Treatment Approach Proposed for Respiratory Distress in COVID-19
March 26, 2020. “What we are hearing from our intensive care colleagues in Europe and in New York is that many of the critically ill patients with COVID-19 are hypercoagulable, meaning that they are clotting off their IVs, and having kidney and heart failure from blood clots, in addition to lung failure,” author Michael Yaffe, a David H. Koch Professor of Science at MIT said in a press release. “We don’t have to make a new drug, and we don’t have to do the same kind of testing that you would have to do with a new agent. This is a drug that we already use. We’re just trying to repurpose it.” …
The hospitals planning to test this approach are Beth Israel Deaconess, the University of Colorado Anschultz Medical Campus, and Denver Health.
(2). April 06, 2020. BIDMC launches clinical trial to assess common anti-clotting medication for treatment of COVID-19-related respiratory failure
APRIL 06, 2020. “Researchers have considered the use of anti-coagulant drugs to reduce ARDS-induced death for two decades. Though the approach has never been widely adopted or formally FDA-approved, a clinical observation made about a subset of patients with COVID-19 induced ARDS made the idea seem newly relevant.
‘We’re hearing anecdotally that a subset of patients with COVID-19 induced ARDS are clotting abnormally around their catheters and IV lines,’ said senior author, Michael B. Yaffe, MD, PhD, an attending surgeon in the departments of Acute Care Surgery, Trauma, and Surgical Critical Care, and in Surgical Oncology at BIDMC. “We suspect these patients with aggressive clotting are will show the most benefit from tPA treatment, and this new clinical trial will reveal whether that’s the case.”
(3). April 06, 2020. Beth Israel Deaconess Medical Center seeking treatment of respiratory failure linked to coronavirus
“Dr. Michael Yaffe, the attending intensive care physician and surgeon at Beth Israel Deaconess Medical Center, is among those treating the sickest COVID-19 patients.
‘These patients, by and large, primarily have a terrible form of lung injury from this virus,’ Yaffe said.
The lung injury is called acute respiratory distress syndrome, or ARDS, and is common in patients with other diseases, but it is much more severe in those who have COVID-19.
Yaffe said ventilators are not having the desired effect on COVID-19 patients who are critically ill and have severe cases of ARDS. He believes blood clots are to blame.
‘Most of the time, what we're seeing is although the lungs can be filled with air at modest pressures, the oxygen isn't being transferred to the blood vessels,’ Yaffe said. ‘These patients are clotting their IVs, they're clotting dialysis catheters (and) they're clotting central lines.’
In response, a few of Yaffee's trainees, who are surgical residents, thought of using an anti-clotting drug, tPA, that has been used for decades, typically to treat heart attack and stroke patients.
(4). Ivermectin: enigmatic multifaceted ‘wonder’ drug continues to surprise and exceed expectations, February 2017
Up until recently, avermectins were also believed to lack antibacterial activity. However, in 2012, reports emerged that ivermectin was capable of preventing infection of epithelial cells by the bacterial pathogen Chlamydia trachomatis, and to do so at doses that could be used to counter sexually transmitted or ocular infections.101 In 2013, researchers confirmed that ivermectin was bactericidal against a range of mycobacterial organisms, including multidrug resistant and extensively drug-resistant strains of Mycobacterium tuberculosis, the authors suggesting that ivermectin could be re-purposed for tuberculosis treatment.
END





Whether the illness is from a virus or not (I give substantial probability to bacterial infection), I felt immediately better taking ivermectin in May. I was half-deaf and the pressure from my ears started to relieve in minutes.
When we got COVID (or whatever) in 2021, we took ivermectin and felt so much better just a couple of hours later. I mean, WAY better...I worked out later that day. Prior to that, I was lying on our made bed, not wanting to move.
Since then, we’ve kept it around. Whenever one of us (or the kids feels sick -- even the “stomach flu,” we take it and voilà! All better. It’s like magic.