The real diseases that were spreading in 2020 were PCR Tests and Hospital Protocols.
It’s not an easy concept to understand or accept. The most confusing facts are the government’s “Gain-of-Function research,” described as an effort to create deadly and contagious “viruses.” Because this type of research clearly exists, the public assumes that there must have been an engineered virus circulating in the public.
Nevertheless, the public now also understands that because the alleged “virus” only became deadly in hospitals, and there is something very wrong with this picture.
I wouldn’t understand things nearly as well if it were not for the Baileys “Farewell to Virology” series. Scientists create chemical compounds in labs with computers. Ralph Baric was not using a scalpel to slice and dice his tiny compounds together. I consider these compounds to be a hybrid between biological and chemical weapons. They are RNA and DNA based chemicals designed to interact with the body's chemistry by using the body’s code of RNA and DNA. They call them “engineered viruses.” Shakespeare would tell you that you can call them a Rose or whatever you want to.
The definition of a virus is a DNA or RNA genome inside a protein shell called a capsid. Although viruses may or may not exist naturally inside a protein shell, nucleic acids do exist. Scientists work to modify these nucleic acids to create disease.
That does not mean these compounds they can escape from labs and circle the globe via human-to-human transmission, however. In order to confirm the existence of their engineered hybrid biological/chemical weapons in the public, scientists falsely confirm a similar sequence to the “engineered virus” using computer programs that slice up and recombine materials into a similar sequence from lung fluid samples containing a large amount of substances.
Scientistss simply ask the computer to divide all of the unidentified materials in lung fluid samples into tiny pieces called “contigs,” then reassemble them to fit a “virus” template. They discard the rest. Whether viruses can be proven to exist or not, a virus has never been isolated and sequenced. There are no legitimate virus sequences. As the parent genetic sequence of SARS-CoV-2 is fraudulent, all PCR tests that confirm the SARS-CoV-2 sequence are meaningless.
Then, scientists, media, and governments trick the public into INJECTING the engineered compounds via something they call a “vaccine.” This is the scam of modern virology that you have witnessed.
mRNA can generate a protein in the human body. This time it was a “spike protein.” The spike protein only had to be inserted into a genetic sequence by the likes of Ralph Baric by typing into a sequence that is a series of numbers and letters. Whoever was running the genetic sequencing software in China closely mirrored this type of sequence. That is all that was required to have fake “virus.” The rest is all smoke and mirrors.
In 2020, PCR tests were used as a tool to confirm a disease in the elderly that never existed. These elderly were subsequently killed by medical professionals in terribly high numbers, and their deaths were in turn falsely blamed on “COVID,” fueling the perception of a false need for deadly and disease-causing mRNA-based vaccines.
As Ralph Baric says: “In virology, historically, attenuated vaccines were generated by gain-of-function studies… Baric believes such research is essential to the development of vaccines and other countermeasures against emerging viruses, a project he has been engaged in for more than 20 years.”
So how does this stuff actually get into your body? Disinformation. Deception. A trick.
Consider Occam’s Razor here, “the problem-solving principle that recommends searching for explanations constructed with the smallest possible set of elements.” Although Occam’s Razor doesn’t always hold, many times the most simple answer is the truth. You know people injected mRNA-based poison. You know “Gain-of-Function Research” had a goal of creating vaccines. You can call mRNA/DNA based poisons a vaccine, a virus, a rose, or whatever.
The transmission was “asymptomatic.” People died in hospitals- even in China where the Plandemic began. Hospitals are supposed to save people’s lives, not kill them. So just think about it.
I don’t want to become too divisive on the “virus/no virus” debate, because people “wake up” at different times. Regardless of your opinion on that, moving on, I think we can all agree that an “engineered virus” story was used as a scapegoat for what can only be described as a mass homicide by the medical profession.
This article is a summary of NPR reporting on nursing homes in 2020. If you read their articles in the hindsight and context of what I just wrote, their reporting will have a fresh meaning to you.
NPR REPORTING ON NURSING HOMES, 2020
March 05, 2020. Trump Administration Announces New Scrutiny Of Nursing Homes
The Centers for Medicare & Medicaid Services is ordering health inspectors to focus on infection-control practices at nursing homes and hospitals, particularly those where coronavirus infections have been identified among patients or in the community, CMS administrator Seema Verma announced Wednesday.
"We are hyperfocused on infection control right now," Verma said. "Our role in this is to say, 'Were there some breaches of protocol? Was this facility following the guidelines that are in place? Was there hand-washing? Were they changing gloves? Were they doing laundry appropriately? Was food handled appropriately?'"
The heightened regulatory attention comes after the deaths of five people who had lived at Life Care Center of Kirkland, Wash. They all had contracted COVID-19, a respiratory illness caused by the new coronavirus. Verma said inspectors would be dispatched to that nursing home to see whether staff there had followed infection-control rules. She noted that the facility was cited for lapses last year, although inspectors subsequently determined the errors had been corrected.
March 15, 2020. The Struggle To Keep Vulnerable Seniors Safe In A Large Coronavirus Cluster
"This epidemic is very scary. You know just because it's just transferring so fast," Fields said. "You got to ride the subways and then everyone's just clustered on you. I'm nervous."
The National Guard is here helping people manage the disruption, distributing food and helping sanitize public areas. On Friday, a new COVID-19 testing facility was established in the suburban community just north of New York City.
For now, the rules for the one-mile radius containment area still allow people to move around and go to work, though federal guidelines urge people in hotspot areas like this to work from home as much as possible.
Fears focus on seniors, nursing homes
As COVID-19 cases in New Rochelle continue to rise, Gov. Andrew Cuomo says he worries most about people like Joyce Collins.
"That is the most dangerous situation posed by this virus, senior citizens, people with a compromised immune system," he said this week.
Many of the deaths in the U.S. are tied to a single senior care facility in Washington state. Cuomo says he hopes to avoid that kind of crisis, so nursing homes across New York state have been ordered to halt all visitation. That means no unauthorized people in or out.
"Right now what my job is to keep residents we care for safe, to keep them happy," said Rita Mabli who runs United Hebrew of New Rochelle. It's a nursing home and assisted living community with roughly 500 residents in the containment area.
All those people now live under strict lockdown. The staff, too, face new hygiene rules designed to keep coronavirus at bay.
"We screen every single staff that's coming into the facility," says Jerome Bagaporo, a nurse who runs United Hebrew's clinical program. "We ask them...do you have any symptoms? Do you have cough, do you have cold?"
As the days pass, Rita Mabli says tensions have risen. Families, some of them living outside the New Rochelle area, are scared and frustrated by the quarantine.
"There are people who are angry no matter what you do," Mabli says. "We've set up Skype and Facebook access so that people who want to visit face-to-face, virtually face-to-face, with their families can use the Skype."
New Rochelle Mayor Noam Abramson is one of the people directly affected by the nursing home lockdown.
"My mother is at United Hebrew presently and my brothers and I are not able to visit her," he said.
March 24, 2020. Spanish Military Finds Dead Bodies And Seniors 'Completely Abandoned' In Care Homes
The Spanish military has found older residents of some care homes "completely abandoned" and even "dead in their beds," Defense Minister Margarita Robles said in a television interview on Monday.
They were found as soldiers disinfected and provided emergency health care services this week to residential homes across the country. Robles did not give an exact figure for the number of dead bodies found by Spanish soldiers.
With more than 39,000 confirmed cases of COVID-19 and 2,800 deaths as of Tuesday, Spain is the second hardest-hit country in Europe.
On Tuesday, 514 new deaths were registered in a 24-hour period, the worst increase since the outbreak began. Retirement homes have been particularly affected.
March 31, 2020. To Stop The Pandemic, Seema Verma Is 'Getting Rid Of A Lot Of Regulations'
In New York City, emergency hospital beds are multiplying — inside tents set up in Central Park, on a hospital ship docked on Manhattan's West Side and in the Javits Convention Center, which now houses about 1,000 beds.
To give the rest of the country similar flexibility in addressing the wave of COVID-19 patients expected to need hospital care soon, the federal government is relaxing a lot of what are usually thought of as safety requirements, says Seema Verma, administrator of the Centers for Medicare and Medicaid Services, and a senior member of the White House Coronavirus Task Force. Hospitals can now operate inside dorms, for example, as well as gyms, schools, and parking lots.
Right now, Verma tells All Things Considered Host Mary Louise Kelly, thousands of civil servants at CMS are moving heaven and earth to make it easier for hospitals to care for patients during the coronavirus crisis. The agency has a huge reach — it runs Medicare, with 60 million enrollees, overseeing provider payments and plans. It also works in partnership with states to administer Medicaid, with 74 million enrollees, and oversees many nursing homes, managing inspections and quality ratings of the facilities.
On Tuesday, Verma spoke with Kelly about how the Trump administration thinks "relaxing safety rules" and easing licensing restrictions might help patients, and why widespread testing continues to be such a problem. The interview has been edited for length and clarity.
These tents we've all watched being pitched in Central Park. Can you give us a concrete example or two of what you envision this actually looking like in other American cities?
Sure. FEMA is doing an incredible job setting up these temporary hospitals in New York and other parts of the country. But we want to empower local communities to also be able to take action and to tap into their local resources. So, for example, hospitals don't need to be thinking about only providing services within their four walls. You know, right now there are surgery centers that are out there — about 5,000 of them across the country. And those surgery centers are not performing elective surgeries. So they have some capacity there, they have medical equipment.
And that could be a place where hospitals say, 'We're going to direct all of our cancer patients there. We're going to perform infusion therapy there.' And so they're allowed to go beyond their four walls. That allows us to also treat patients that may not have just [coronavirus] — there are people out there that need medical care, whether it's cancer treatment or some other type of care. It allows facilities to create separation, so you can put infected patients in one place and coronavirus in another — it allows them that flexibility to triage patients. They could even do that outside of the emergency room — in the parking lot — and figure out where people need to go.
This is still up to states — they can decide what they want to do — but your goal is to kick the door open and make this easier for them?
That's exactly it. We are getting rid of lots of different regulations. One is this concept of hospital without walls. So a hospital that may be located close to a college university — a lot of the universities have gone virtual, so the dorms are empty. And they could say, 'We're going to provide services in these dorms' and they can already start working on that to prepare for the surge. And that way, the hospital can focus on the most complex patients. The other thing that we're doing for hospitals is giving them more flexibility to boost their workforce. There are a lot of rules and regulations in terms of credentialing, and we're relaxing those a little bit. They still have to defer to their state law, but the federal government's not getting in the way of that.
This is things like relaxing supervision of residents and nurse practitioners and others?
Exactly. And then letting some of those paraprofessionals — whether it's physician assistants or nurse anesthetists — to allow them to operate at the top of their license. So, for example, a nurse anesthetist. They can perform or assist in a surgery — putting somebody under — and they don't necessarily need to be supervised by an anesthesiologist. They can do that and their license would allow them, but there [are] sometimes federal barriers that don't allow them to do that. And that becomes really important, because you can imagine when you're worried about the workforce, you may want to have your anesthesiologist in the ICU and have the nurse anesthetist in a different location, maybe performing a lower-level surgery. So it just allows us to really maximize the entire workforce, to make sure that they can deal with the surge in patients.
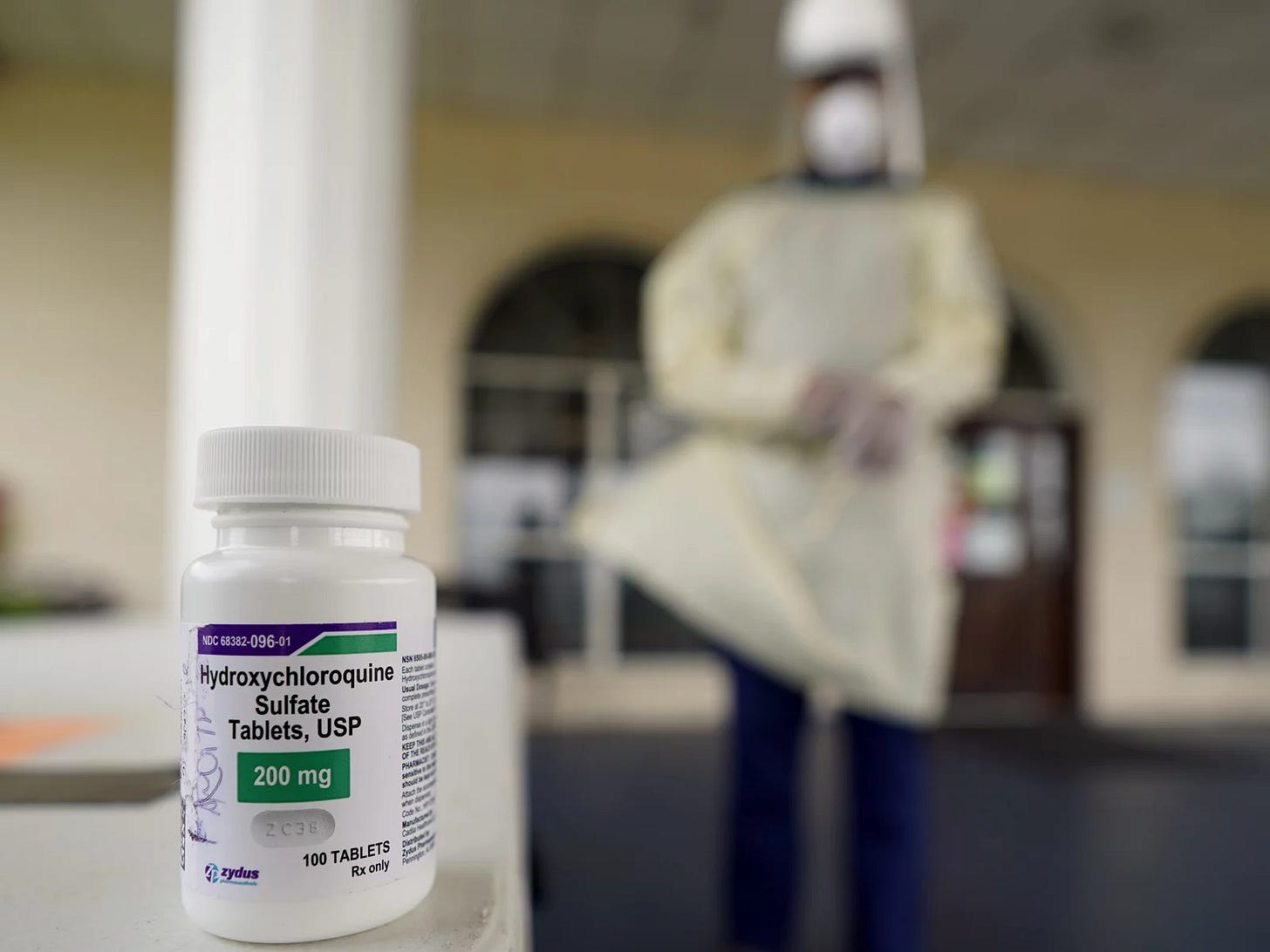
April 10, 2020. COVID-19 Patients Given Unproven Drug In Texas Nursing Home In 'Disconcerting' Move
Concern is mounting after a doctor at a Texas nursing home started giving the anti-malaria drug hydroxychloroquine to dozens of elderly patients diagnosed with COVID-19 and tracking the outcomes in what he's calling an "observational study."
Use of the drug to treat coronavirus infections has set up a heated debate between the Trump administration and leading health experts over its efficacy against COVID-19.
President Trump has been an enthusiastic champion of hydroxychloroquine, calling it a "game-changer." But some of the nation's most respected health officials have said there is insufficient evidence showing that the 80-year-old drug, which is typically used to stave off malaria or treat lupus and rheumatoid arthritis, is a viable treatment in battling the new virus.
The Food and Drug Administration has not approved the drug for the treatment of COVID-19. The U.S. National Institutes of Health is currently tracking clinical trials of the drug. Additionally, the University of Minnesota is undertaking a trial and Columbia University is as well. Results are not expected for weeks or months.
The controversial decision to administer hydroxychloroquine at The Resort at Texas City over the last few days was made by Robin Armstrong, a physician and medical director of the nursing home.
"It's actually going well. People are getting better," Armstrong told NPR, adding that after just a handful of days, some of the 39 patients on the medication are showing signs of improvement.
But scientists argue that relying on observational, uncontrolled evidence can be misleading and that the only way to truly prove a drug is working is through carefully controlled clinical trials. And, contrary to Armstrong's assertion that hydroxychloroquine "has virtually no side effects," it is known to have serious negative health impacts. That is why so many in the medical community worry about prescribing it without such proof.
April 14, 2020. Fla. Governor Says National Guard Ramping Up Coronavirus Testing In Nursing Homes
DeSantis said the four-person National Guard "strike teams" have already been sent to 93 such long-term-care facilities, where a total of 962 positive cases have been discovered. But he said he wants to further expand testing.
"I am directing the Florida National Guard to create more strike teams to significantly ramp up testing in long-term-care facilities," he said at a news conference in Tallahassee.
DeSantis said the surge in testing was needed to identify asymptomatic carriers of the novel coronavirus, especially among staff members who might be unwittingly spreading it at facilities where the high number of elderly and immunocompromised residents make COVID-19 particularly deadly.
April 14, 2020. Half Of Virginia's Coronavirus Outbreaks Are In Long-Term Care Facilities
A new data breakdown shows more than half of reported COVID-19 outbreaks in Virginia are in long-term care facilities, like nursing homes and assisted-living facilities. As of Tuesday morning, 56 out of 102 reported outbreaks had occurred in these settings.
Officials declined to identify the names of the facilities where more than 600 people have been infected. The Virginia Department of Health (VDH) says according to policy, it won't release these names unless the individual facilities themselves give permission.
A spokesperson for VDH's public records office cited a section of Virginia code barring the state health Commissioner or local health districts from releasing the information to the public. Meanwhile, several other states like Minnesota and Oklahoma are releasing the names of long-term care facilities with confirmed cases.
In Florida, the Miami Herald says it plans to sue the state to get the names of elder-care facilities with coronavirus cases. "Anyone with a relative in an elder-care facility has a right to know if their loved ones are at risk so they can make an informed decision about their care," said Herald publisher Aminda Marqués González.
Dr. Laurie Forlano, Deputy Commissioner for Population Health at the Virginia Department of Health, detailed a recent outbreak in a long-term care facility during a press briefing Monday but was careful not to name the specific location. "Staffing continues to be an issue, and that was true here as well," Forlano said.
Dr. Danny Avula, Director of Richmond City and Henrico County Health Districts, confirmed during a press conference Tuesday that 15 long-term care facilities across the two jurisdictions have confirmed COVID-19 cases. That includes the Canterbury Rehabilitation and Healthcare Center in Henrico County, where 45 patients have died after testing positive for the coronavirus.
"This is a disease that spreads at high rates in an elderly, vulnerable population," Avula said. "What we're seeing in congregate care facilities is that asymptomatic spread is an even more significant part of transmission than we realized."
April 17, 2020. West Virginia Aims To Test All Nursing Home Residents, Workers For COVID-19
Amid growing concern about the well-being of residents of elder care facilities, West Virginia officials are preparing to test every nursing home resident and worker in the state for the new coronavirus.
Gov. Jim Justice has issued an executive order directing state health officials and the National Guard and to conduct the tests, including retesting those who've previously been checked for the virus.
"Our nursing homes, we all know, are the most vulnerable of all of our people," Justice said during a briefing on Friday. "This disease has a way of attacking the elderly."
The decision follows outbreaks at care centers nationwide, including multiple positive tests at a facility in Jackson County, W.Va., this week.
Justice expressed frustration at incomplete testing and inconsistent information he said was coming from nursing homes where outbreaks of the virus have occurred.
"I'm sick and tired of listening to the discrepancies," he said. "We've gotta go back and redo everybody."
A spokesman did not immediately respond to a request from NPR for data on the number of tests that will be administered in West Virginia, and information about the state's testing capacity.
No other state has required tests "on the scale of West Virginia as far as we are aware," said James Nash, a spokesman for the National Governors Association.
Elder care centers have been a major focus of concern as numerous outbreaks and deaths have occurred at such facilities. In Florida, the National Guard also has been brought in to help ramp up testing at nursing homes and assisted living centers. In Virginia, where more than half of reported outbreaks have been at long-term care centers, Gov. Ralph Northam recently set up a nursing home task force designed to help mitigate the spread of the virus.
April 20, 2020. Discharging COVID-19 Patients To Nursing Homes Called A 'Recipe For Disaster'
In some parts of the U.S., the desperate need to slow the spread of the coronavirus is coming into conflict with the scramble to find more hospital beds.
Nursing homes have been the sites of some of the earliest — and deadliest — outbreaks of COVID-19. Some people who run such facilities are understandably leery of accepting new patients who might spread the virus.
Nonetheless, some of the largest states are now ordering nursing homes to accept patients who have been discharged from the hospital but are still recovering from COVID-19.
These state directives have been strongly condemned by the Society for Post-Acute and Long-Term Care Medicine. Dr. Sabine von Preyss, chief medical officer for Avalon Health Care Group and president of the society's Washington state chapter, says that a distinction must be made between nursing homes that have suffered COVID-19 outbreaks and those that are still virus-free.
"The question is, should we be forced to introduce a disease with such deadly potential into a population that has been sheltered?" says von Preyss. "And my experience tells me that would be ill-advised."
Also, it won't even help overcrowded hospitals, says Dr. Michael Wasserman, who heads the California Association of Long Term Care Medicine.
"If you push folks out of the hospitals to make space and you push them into nursing homes a couple weeks later," Wasserman says, "for every one of those you send to the nursing home, you may get 20 back in the hospital."
April 20, 2020. Nursing Home COVID-19 Reporting Rules To Be Strengthened
After shocking instances of nursing homes failing to disclose the existence and extent of COVID-19 cases within their facilities, the federal government will require nursing homes to inform residents, their families and representatives when residents or staff contract the illness.
The Centers for Medicare & Medicaid Services announced Sunday night that notification must come within 12 hours of a confirmed single case of COVID-19. Residents, families and representatives must also be told when three or more individuals develop respiratory symptoms within a 72-hour period.
The new rules also require nursing homes to report COVID-19 cases directly to the Centers for Disease Control and Prevention as the CDC works to build a nationwide database of the occurrence of the illness. Nursing homes are already required to report such data to state and local public health officials.
"Nursing homes have been ground zero for COVID-19," Centers for Medicare & Medicaid Services Administrator Seema Verma said in a statement announcing the new rules, which she described as an effort to provide "transparent and timely information to residents and their families."
May 11, 2020. New Jersey Investigates State's Nursing Homes, Hotbed Of COVID-19 Fatalities
Coronavirus fatalities in nursing homes and other long-term care facilities account for at least one-third of the deaths in 26 states.
In New Jersey's nursing homes, the coronavirus has proved especially deadly: 53% of the more than 9,000 people who have died from COVID-19 as of Monday in the state were long-term care patients or staff.
Now, New Jersey Attorney General Gurbir Grewal has opened an investigation into possible misconduct at those facilities.
In addition to the high infection and death rates, Grewal says there were other issues that prompted the launch of the investigation.
"It was also the reporting that we were seeing and hearing about how bodies were being handled, about the lack of communication and transparency with families," he tells All Things Considered. "Because of all of those reasons, we felt an obligation to look for answers and to figure out if something went wrong, what happened, and if there are people to be held accountable, who those people are."
In one case, 17 bodies were discovered last month in a makeshift morgue at a facility in Andover, N.J.
In the first few days after Grewal's office asked the public to report any leads on possible misconduct, he says more than 200 tips poured in.
May 21, 2020. Ideal Nursing Homes: Individual Rooms, Better Staffing, More Accountability
Nursing homes were not on our minds much before the COVID-19 pandemic. Then their residents began dying by the thousands.
While there are no definitive figures, nursing home residents and staff appear to account for about one-third of the roughly 90,000 COVID-19 related deaths in the U.S., according to The New York Times. Those figures may be low because some states do not report such figures and the CDC is just beginning to collect them.
May 19, 2020. Pennsylvania Health Secretary Defends 'Universal' Nursing Home Testing Plan
Dozens have died of COVID-19 at the Brighton Rehabilitation and Wellness Center in Brighton Township, Pa., pictured on May 12. Pennsylvania's health secretary defended the state's plan to test every resident and staffer at every nursing home.
Of the 4,624 people who have already died of the coronavirus in Pennsylvania, at least two-thirds of them were associated with nursing homes or other long-term care facilities.
Last week Pennsylvania's health department said it's "executing a robust universal testing strategy" for the more than 80,000 residents and 10,000 staffers at 1,900-plus facilities.
But in the week since the announcement, some long-term care facilities have been left confused and saying they haven't been given enough guidance. SpotlightPA reported on some weaknesses in the current guidance: that it calls for voluntary compliance; recommends full testing only at facilities with confirmed or suspected COVID-19 cases; and excludes long-term care facilities that aren't nursing homes.
June 1, 2020. Nearly 26,000 Nursing Home Residents Have Died From COVID-19, Federal Data Show
Newly released data from the U.S. government show that nearly 26,000 nursing home residents have died from COVID-19 and more than 60,000 have fallen ill. These figures, however, don't account for all nursing homes across the country.
According to the Centers for Medicare and Medicaid Services, known as CMS, about 80% of nursing homes nationwide reported data to the CDC as is now required. The remaining 20% could face fines if they don't comply.
CMS Administrator Seema Verma told reporters on a conference call Monday that the data has limitations: Some facilities have reported cumulative figures, and some have reported weekly. She said she expects the discrepancies will even out over time. The figures will be publicly available Thursday on a government website called Nursing Home Compare.
Verma also said CMS had found that the nursing homes with the lowest ratings had some of the worst outbreaks of COVID-19. In March, CMS ordered states to inspect nursing homes for proper infection control. But figures released Monday show that nationwide, a little over half of those inspections have been done, with Nevada completing 100 percent of inspections and West Virginia completing around 11 percent.
States that do not finish all of the required infection inspections by the end of July could face having to forfeit some of their funding under the coronavirus aid package known as the CARES Act. That money could be redistributed among states that are in compliance with the requirement.
CMS also announced Monday that it will be stepping up fines for nursing homes that fail to sufficiently control infections. Nursing homes that have previously been cited for lax infection control could receive fines ranging from $5,000 to $20,000.
June 9, 2020. Banned From Nursing Homes, Families See Shocking Decline In Their Loved Ones
Family members often are an integral part of the care residents in nursing homes receive. They make sure meals are being eaten, clothes are being changed. They also offer invaluable emotional support.
Without it, the consequences can be dire. NPR spoke to several families about what's happened since the mid-March visitor ban. All reported seeing shocking declines in their loved ones.
Advocates for residents say it's time to rethink the outright ban.
Nursing homes can permit visitors for "compassionate situations." But that's usually interpreted as meaning end-of-life visits. Robyn Grant, public policy director for the National Consumer Voice for Quality Long-Term Care, says that compassionate care needs to be interpreted more broadly.
"Residents are declining mentally, physically," she says. "We think that those situations are times when family members should be permitted."
Luann Thibodeau has seen that decline in her husband. She used to bring dinner for him every night except Tuesdays when she goes to Bible Study. She says that as his multiple sclerosis has worsened, he's become increasingly disinterested in food.
August 4, 2020. Nursing Home Residents Moved Out To Make Way For COVID-19 Patients
In some nursing homes, 100% of the residents are positive for the coronavirus. That's by design. These facilities have volunteered to devote part or all of their buildings exclusively to treating COVID-19 patients, who bring in more government money. But to make room for them, the original residents can be forced out of the places they've called home.
"They had no TVs, no radios and no phones," Oliver says. "So there was no contact to the outside world, period."
Hamilton deteriorated after the move and died on June 4.
Sudden relocations can be dangerous for older adults, says Tracy Greene Mintz, a licensed clinical social worker who focuses on a well-documented syndrome called transfer trauma.
"The shorter-term consequences are disability and death," Mintz says.
August 4, 2020. As COVID-19 Numbers Improve, Florida Considers Nursing Home Visits
It's been more than four months since Florida halted all outside visits to nursing homes and assisted living facilities in an effort to protect residents from COVID-19. The policy has helped keep elderly residents safe, but DeSantis said he's heard from many who were distressed that they couldn't be with family members in their final moments. "It leaves a mark," he said.
DeSantis said he wants to begin allowing people who test positive for antibodies to visit family members in long-term care facilities. People with antibodies, he said, aren't at risk of catching or further spreading the virus. He's appointed a committee of advocates and officials to look at other measures to allow family members to visit nursing homes.
August 26, 2020. The United States' Pre-Existing Conditions
So how is it that the richest nation in the world has been laid low by a virus only a few dozen nanometers in size?
To answer this question, we talked to Ed Yong, a science writer for the Atlantic who has spent the past seven months covering COVID-19. In his September cover story for the magazine, titled "How the Pandemic Defeated America," he says it's the inequities that have been with us for generations that made the U.S. so vulnerable to the virus. Below is an excerpt from our conversation, which has been edited and condensed for clarity.
The overarching thesis of this piece is that SARS-CoV-2 is a new virus. But all the problems that have emerged during the pandemic are not new. They were predictable and preventable. They had been discussed beforehand, and just ignored and left to fester. And we are now paying the price for that.
And the same could be said for nursing homes. The fact that nursing homes account for more than 40 percent of deaths from COVID-19 in America is truly shameful. I think it reflects our attitudes to the oldest among us— people who we should be giving respect and care to, but instead who we often neglect. And this isn't to say that like all nursing homes are bad, but it is to say that they are underfunded and understaffed, and that they were not the recipient of extra disproportionate support and attention when this pandemic started spreading. And they should have been. The people who work and live in those nursing homes and other long term care facilities paid the price for that neglect.
October 22, 2020. For-Profit Nursing Homes' Pleas For Government Money Brings Scrutiny
Nursing homes have been overwhelmed by the coronavirus. Residents account for more than a quarter of all COVID-19 deaths nationwide. The industry says that facilities have also been overwhelmed by costs, and they're asking for billions in aid from the federal government.
But recent studies suggest that for-profit ownership may have endangered residents by skimping on care, while funneling cash to owners and investors.
"They're trying to make money," she says. "And the main way to make money is to keep labor costs low."
"It's a deliberate strategy as part of making money," Harrington says. "And that means that they're leaving their residents unprotected."
Illinois records show that some of their rural facilities have had few if any cases of COVID-19. General Counsel Fred Frankel says they followed all federal and state guidelines. But the homes that did have outbreaks appeared helpless to stop them. A handful reported almost as many infections as they had beds. Just 4 homes accounted for almost 80 deaths.
When the crisis hit, he says, nursing homes didn't have the reserves to deal with it. "Nursing homes, for the most part across the country, were underfunded coming into the pandemic."
Parkinson means underfunded by the government, especially Medicaid. In fact, most nursing home revenue comes from the taxpayers, through Medicaid and Medicare.
END























Exactly. I am so tired of the people who say that they had some new bug that was so different. Losing taste and smell is common with sinus infections and common cold, but people nowadays act like it’s the strangest symptom in the universe.
Charles; I think you've managed to put the pieces of the puzzle together faster than most of us. Great job! Let's see how the big-wigs in the Not-a-Freedom movement respond. That will certainly be a big tell on who is controlled opposition. The one solid guy is still Dr. Yeadon.